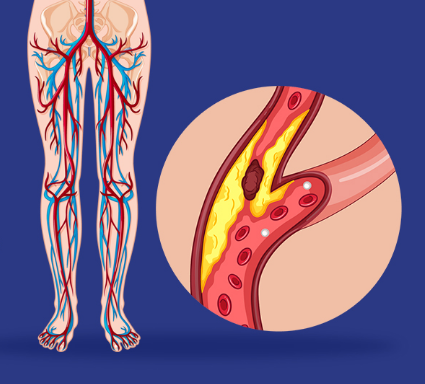
Peripheral artery disease (PAD) is plaque (atherosclerosis) buildup in your leg arteries. This makes it harder for your blood to carry oxygen and nutrients to the tissues in those areas. PAD is a long-term disease, but you can improve it by exercising, eating less fat and giving up tobacco products.
How common is peripheral artery disease?
PAD is common, affecting between 4.1 to 5 crore Indians. Actual numbers are probably higher as most of the times its underdiagnosed disease. In PGIMER, We usually see more than 100 patients OPD everyday suffering with PVD related issues.
How does peripheral artery disease affect body?
The typical symptom of PAD is called claudication, a medical term for pain in your leg that starts with walking or exercise and goes away with rest. The pain occurs because your leg muscles aren’t getting enough oxygen.
The dangers of PAD extend well beyond difficulties in walking. Peripheral artery disease increases the risk of getting a nonhealing sore in your legs or feet. In cases of severe PAD, these sores can turn into areas of dead tissue (gangrene) that can sometimes lead to amputation of toes, foot or leg.
What are the stages of peripheral artery disease?
Healthcare providers can use two different systems — Fontaine and Rutherford — to assign a stage to your PAD. The Fontaine stages, which are simpler, are:
I: Asymptomatic (without symptoms).
IIa: Mild claudication (leg pain during exercise).
IIb: Moderate to severe claudication.
III: Ischemic rest pain (pain in your legs when you’re at rest).
IV: Ulcers or gangrene.
SYMPTOMS AND CAUSES
The first symptom of PAD is usually pain, cramping or discomfort in your legs or buttocks. This happens when you’re walking and goes away when you take rest.
What are the typical symptoms of peripheral artery disease?
A burning or aching pain in your feet and toes while resting, especially at night while lying flat.
Cool skin on your feet.
Redness or other color changes of your skin.
More frequent skin and soft tissue infections in your feet or legs
Toe and foot sores that don’t heal.
Half of the people who have peripheral vascular disease don’t have any symptoms. PAD can build up over a lifetime. Symptoms may not become obvious until later in life. For many people, symptoms won’t appear until their artery narrows by 60% or more.
Talk to a Vascular surgeon if you’re having symptoms of PAD so they can start treatment as soon as possible. Early detection of PAD is imperitive for starting timely treatment to avoid severe complications like a heart attack or stroke.
What are the complications of peripheral artery disease?
Without treatment, people with complicated PAD may need an amputation — the removal of part or all of your foot or leg (rarely your arm), especially in people who also have diabetes.
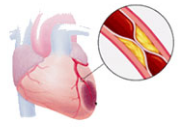
Because your body’s circulatory system is interconnected, the effects of PAD can extend beyond the affected limb. People with atherosclerosis of their legs often have it in other parts of their bodies.
What is the most common cause of peripheral artery disease?
Atherosclerosis that develops in the arteries of your legs — or, less commonly in your arms — causes peripheral arterial disease. Like atherosclerosis in your heart (coronary) arteries, a collection of fatty plaque in your blood vessel walls causes peripheral vascular disease. As plaque builds up, your blood vessels get narrower and narrower, until they’re blocked.
What are the risk factors for peripheral artery disease?
Tobacco use is the most important risk factor for PAD and its complications. In fact, 80% of people with PAD are people who currently smoke or used to smoke. Tobacco use increases the risk for PAD by 400%. It also brings on PAD symptoms almost 10 years earlier.
Compared with non-smokers of the same age, people who smoke and have PAD are more likely to have heart attack or stroke and have a limb amputation.
Regardless of your sex, you’re at risk of developing peripheral arterial disease when you have one or more of these risk factors:
Using tobacco products (the most potent risk factor).
Having diabetes
Being age 50 and older.
Having a personal or family history of heart or blood vessel disease.
Having high blood pressure (hypertension)
Having high cholesterol (hyperlipidemia).
Having abdominal obesity.
Having a blood clotting disorder.
Having kidney disease (both a risk factor and a consequence of PAD).
DIAGNOSIS AND TESTS
A vascular surgeon or vascular care provider(interventional radiologist/cardiologist) will perform a physical exam and review your medical history and risk factors. They may order non-invasive tests to help diagnose PAD and determine its severity. If you have a blockage in a blood vessel, these tests can help find it.
Ankle-brachial index (ABI).
Pulse volume recording (PVR).
Vascular ultrasound.
You may also need an invasive test called an angiogram to find artery blockages.
MANAGEMENT AND TREATMENT
Can peripheral artery disease be reversed?
Yes. Some studies have shown that you can reverse peripheral vascular disease symptoms with exercise and control of cholesterol and blood pressure.
With early diagnosis, lifestyle changes and treatment, you can stop PAD from getting worse.
Lifestyle changes
Quit using tobacco products- Ask your physian about smoking cessationprograms.
Eat a balanced diet that’s high in fiber and low in cholesterol, fat and sodium. Limit fat to 30% of your total daily calories. Saturated fat should account for no more than 7% of your total calories. Avoid trans fats, including products made with partially hydrogenated and hydrogenated vegetable oils.
Exercise-Start a regular exercise program, such as walking. Walking can help treat PAD. People who walk regularly can increase the distance they’re able to walk before their legs hurt.
Manage other health conditions, such as high blood pressure, diabetes or high cholesterol.
LIVING WITH IT
It’s important to take good care of your feet to prevent nonhealing sores. Foot care for people who have PAD includes:
Wearing comfortable, appropriately fitting shoes.
Inspecting your legs and feet daily for blisters, cuts, cracks, scratches or sores. Also check for redness, increased warmth, ingrown toenails, corns and calluses.
Not waiting to treat a minor foot or skin problem.
Keeping your feet clean and well moisturized. (Don’t moisturize an area with an open sore.)
Cutting your toenails after bathing, when they’re soft. Cut them straight across and smooth them with a nail file.
In some cases, your healthcare provider may refer you to a vascular surgeon (foot expert) for specialized foot care – especially if you have diabetes.
When should one see Vascular Surgeon or Vascular Specialist?
Contact your healthcare provider if you:
Get a bad infection in a sore on your foot. The infection can expand into your muscles, tissues, blood and bones. If your infection is severe, you may need to go to the hospital.
Can’t walk around enough to do normal activities.
Have pain in your legs when you’re resting. This is a sign of poor blood flow.
The author is Vascular Surgeon, at PGIMER Chandigarh















