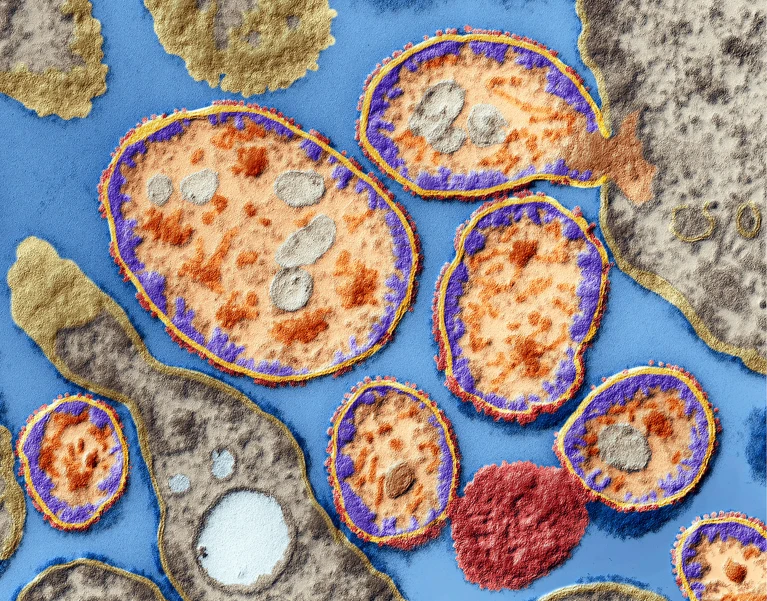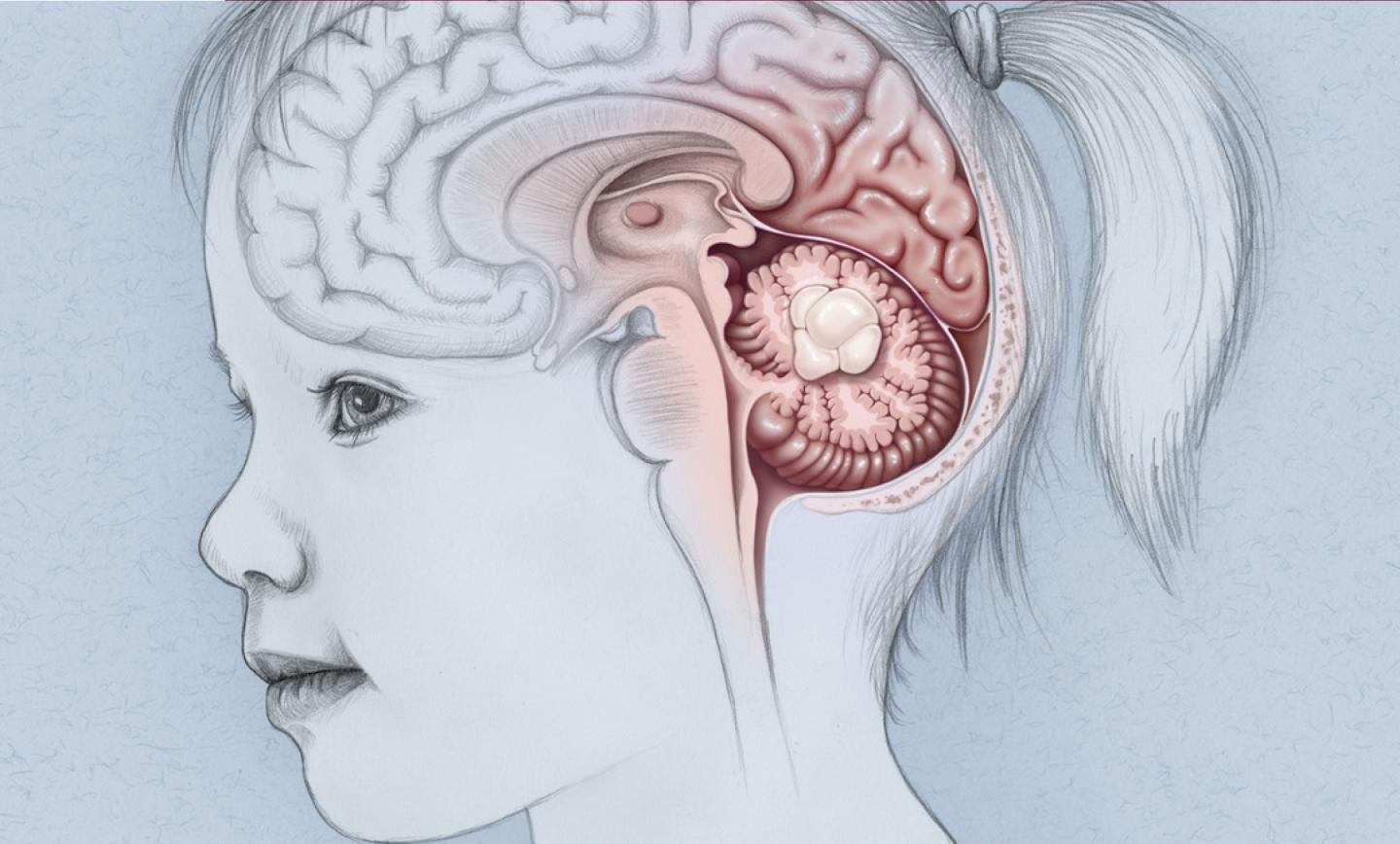
Pediatric brain tumors are among the most challenging and complex medical conditions that affect children. These tumors can arise from various types of cells within the brain and central nervous system, leading to a diverse array of symptoms, underlying causes, and treatment strategies. The symptoms of pediatric brain tumors can vary widely depending on the tumor’s size, location, and rate of growth. Common symptoms include persistent headaches, nausea, vomiting, balance and coordination difficulties, vision or hearing changes, and cognitive or behavioral alterations. In infants, symptoms might be more subtle, such as an increase in head size, irritability, or developmental delays. Seizures are another critical symptom that may indicate the presence of a brain tumor. These symptoms often result from the tumor exerting pressure on surrounding brain tissues or obstructing the normal flow of cerebrospinal fluid, leading to increased intracranial pressure.
The causes of pediatric brain tumors are multifaceted and not entirely understood. Genetic factors play a significant role in some cases. Environmental factors, though less clearly defined, are also under investigation. Exposure to ionizing radiation is a known risk factor, and there is ongoing research into the potential impacts of other environmental exposures, such as certain chemicals and infections. However, for the majority of pediatric brain tumors, no definitive cause can be identified, making it a complex interplay of genetic predisposition and environmental influences.
Treatment for pediatric brain tumors is equally complex and requires a multidisciplinary approach involving neurosurgeons, oncologists, radiologists, and other specialists. The primary treatment modalities include surgery, radiation therapy, and chemotherapy, often used in combination. In some cases, complete resection is achievable, leading to a better prognosis, but in others, the tumor’s location may limit the extent of surgical removal. Advanced surgical techniques, including minimally invasive approaches and intraoperative imaging, have improved outcomes and reduced complications. Radiation therapy, using high-energy beams to target and destroy tumor cells, is typically employed when complete surgical removal is not feasible or as an adjunct to surgery. In young children, however, radiation therapy poses significant risks to developing brain tissue, potentially leading to long-term cognitive and developmental impairments. Therefore, newer techniques like proton beam therapy, which can more precisely target tumors while sparing surrounding healthy tissue, are being increasingly utilized.
Chemotherapy, the use of drugs to kill cancer cells, is another cornerstone of treatment, particularly for certain types of brain tumors like medulloblastomas and high-grade gliomas. However, the blood-brain barrier, a protective shield around the brain, can limit the effectiveness of some chemotherapy agents, necessitating the development of new delivery methods and drugs that can penetrate this barrier. Emerging therapies, including targeted therapy and immunotherapy, are showing promise in treating pediatric brain tumors. Targeted therapy involves drugs that specifically target genetic mutations or pathways driving tumor growth, offering a more personalized and less toxic treatment option. Immunotherapy leverages the body’s immune system to recognize and attack cancer cells and is an area of active research in pediatric oncology.
The treatment of pediatric brain tumors also involves addressing the long-term effects of both the disease and its treatment. Survivors often face challenges such as cognitive impairments, physical disabilities, and emotional and psychological issues. Rehabilitation services, including physical, occupational, and speech therapy, play a crucial role in helping children regain lost skills and achieve their developmental potential. Educational support is also vital, as cognitive impairments can affect academic performance and learning abilities. Psychosocial support for both the child and their family is essential, as the diagnosis and treatment of a brain tumor can be a traumatic and life-altering experience.
Final Thoughts
Pediatric brain tumors present a formidable challenge due to their diverse symptoms, complex causes, and multifaceted treatment approaches. Advances in surgical techniques, radiation therapy, chemotherapy, and emerging therapies are improving outcomes, but the journey for affected children and their families remains arduous. A comprehensive, multidisciplinary approach that includes medical treatment, rehabilitation, and psychosocial support is crucial in addressing the myriad needs of these young patients and helping them lead fulfilling lives.
The author is the MBBS , MD (Neonatology and Pediatrics) Apollo Cradle & Children’s Hospital- Moti Nagar, New Delhi.