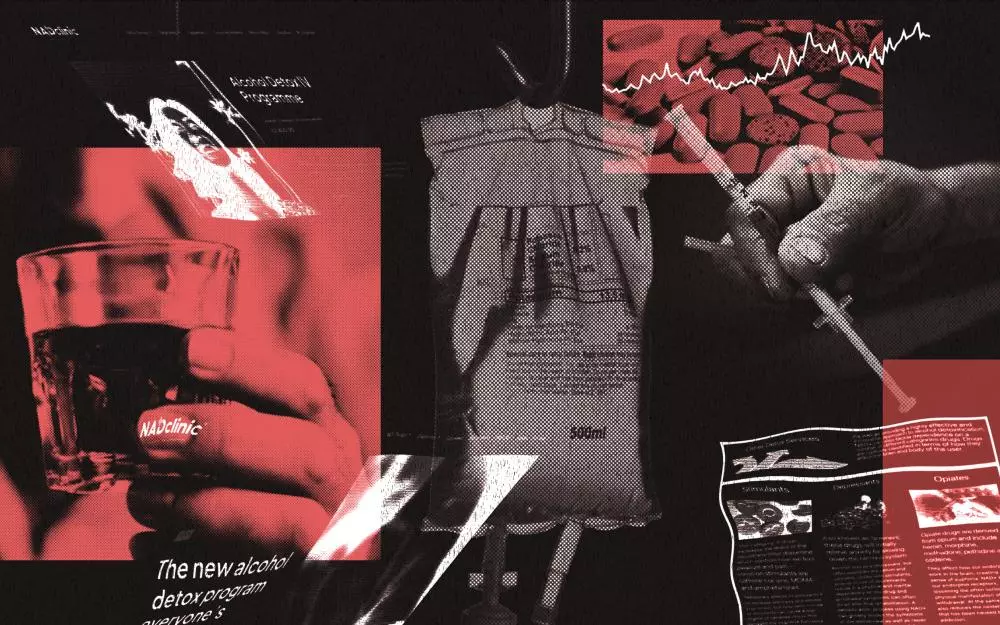
In recent years, NAD+ (nicotinamide adenine dinucleotide) has gained significant popularity, particularly in wellness circles, with claims of reversing aging, boosting cognitive function, and aiding addiction recovery. Its surge in demand has attracted A-listers like Kendall Jenner and Joe Rogan, who publicly support its benefits. However, NAD+ infusions, touted as a “miracle” treatment for substance misuse, have raised concerns within the medical community, with many experts questioning their efficacy, ethicality, and safety.
The treatment involves infusing NAD+, a coenzyme derived from vitamin B3, into the bloodstream, with promises of curing addiction by reducing withdrawal symptoms, repairing damaged cells, and potentially reversing the effects of substance abuse. Despite its celebrity endorsements and the increasing number of clinics offering this treatment in the UK, research and clinical evidence to support these claims remain largely inconclusive. Dr. Michael Sagner, a clinical adviser and expert in NAD+, dismisses the notion of NAD+ being an effective treatment for addiction, labeling it as “complete nonsense.”
Experts argue that the treatment lacks sufficient scientific backing, with no clinical trials demonstrating its effectiveness in treating substance misuse or addiction. The claims made by many UK clinics, some of which are registered with the Care Quality Commission (CQC), suggest NAD+ can detoxify the body, alleviate cravings, and improve mental clarity. These assertions are not only unsupported by robust evidence but also pose potential risks to vulnerable patients undergoing addiction treatment. The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) has even taken action against clinics promoting NAD+ for medical purposes, as it is not licensed for such treatments.
The origins of the claims about NAD+ lie in its supposed role in cellular repair and energy production. NAD+ is naturally present in all cells and has been associated with DNA repair and the regulation of energy. Depletion of NAD+ levels is thought to contribute to aging and degenerative diseases, with proponents arguing that replenishing NAD+ could reverse damage and improve overall health. However, the studies supporting these claims are sparse, with much of the existing research limited to animal studies or small, unregulated trials.
While NAD+ has some scientific merit in specific contexts—such as in energy production and cellular repair—its use as an addiction treatment is speculative at best. Many addiction specialists caution against relying on NAD+ infusions as a primary treatment for addiction, especially when no conclusive evidence exists to show that it helps with withdrawal symptoms or long-term recovery. In fact, experts like Professor Harry Sumnall of Liverpool John Moores University stress that NAD+ infusions can be dangerous if used as a substitute for proven detoxification methods, which address the complex physiological and psychological aspects of addiction.
Furthermore, some of the claims made by clinics are highly questionable. For instance, some facilities have marketed NAD+ infusions as a standalone solution for detox, offering “affordable alternatives to rehab” with success rates as high as 90%. These promises not only mislead patients but also undermine the importance of comprehensive addiction treatment, which typically involves a combination of medical care, psychological support, and long-term rehabilitation.
In a disturbing trend, some clinics have even marketed NAD+ infusions alongside other unproven treatments, such as ketamine, which could lead to even greater health risks for patients struggling with addiction. The fact that these clinics often operate with minimal regulatory oversight further compounds the issue, making it difficult for patients to discern between legitimate medical treatments and exploitative wellness fads.
The MHRA’s stance on NAD+ infusions is clear: without approval as a licensed medicine, claims regarding its ability to treat addiction or other medical conditions are illegal. This has led to some clinics modifying their marketing strategies in the wake of regulatory action, yet others continue to sell NAD+ as a quick fix for addiction, often without fully disclosing the lack of scientific evidence to back their claims.
There is also the issue of the high cost of NAD+ infusions, which can range from £370 for a basic protocol to over £2,800 for a multi-session detox program. These treatments are often sold by wellness companies or private clinics and may not be covered by insurance, making them accessible only to those who can afford the steep prices. This creates a concerning divide in access to addiction treatments, with many individuals in need of evidence-based care being drawn toward expensive, unproven alternatives.
While NAD+ may have some potential as a wellness product, its use as an addiction treatment is deeply problematic. The focus on celebrity endorsements and unregulated wellness clinics only serves to perpetuate the myth that NAD+ can miraculously cure addiction, despite the glaring lack of scientific validation. For those struggling with substance misuse, it is crucial to seek out medically approved, evidence-based treatments rather than place trust in costly, unproven infusions.
In conclusion, the rise of NAD+ infusions in the UK as a treatment for addiction highlights the growing trend of unregulated wellness products being marketed as miracle cures. Despite its widespread promotion and celebrity backing, NAD+ infusions remain unproven and unlicensed for addiction treatment, with experts warning that they could pose serious health risks. Patients in need of addiction recovery should prioritize evidence-based treatments that are backed by clinical research and guided by medical professionals, rather than falling victim to exploitative marketing tactics.