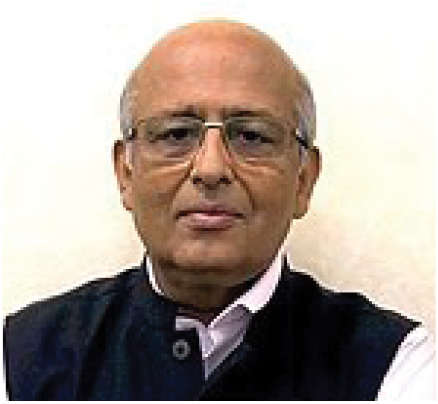
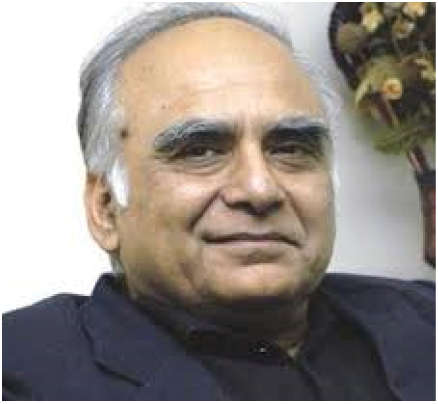
New Delhi: What is in the placebo? Is the recipient of a placebo aware of it? Can a person who has volunteered for the placebo get the Covid vaccine? These are some important questions which are on everyone’s minds as people in certain corners of the world start to receive the Covid vaccine—and others hope to do so soon. Dr Shaheed Jameel, virologist and director of the Trivedi School of Biosciences at Ashoka University, and Dr N.K. Ganguly, former Director General, ICMR, respond to these pressing questions in an exclusive interview with The Daily Guardian.
Q. What is the difference between a placebo and a vaccine?
Dr Jameel: A placebo is something other than the vaccine being tested. Mostly, it is a saline solution but the vial looks exactly the same as the vaccine, so that no one, including the one giving the injection, knows whether they are giving the vaccine or placebo. This is called blinding in the trial.
Dr Ganguly: A placebo is another vaccine, not normal saline, so that they also benefit and they also get some local reaction. Both are packed in a similar vial and injected in a similar volume. After the injection, they have to wait for at least 30 minutes.
Q. How can a volunteer know whether he/she has taken a placebo or a vaccine for Covid-19?
Dr Jameel: Take an antibody test. If positive, you got the vaccine. If not, you got the placebo. But the test may not be positive after the first shot. However, it should definitely be positive after the second shot.
Q. Do you think if a person takes a placebo, he/she can’t take the vaccine? If no, why?
Dr Jameel: A person taking the placebo is like taking nothing. They can take the vaccine and should be the first ones to get it as they volunteered for the trial without knowing whether the vaccine would work or not or whether it is safe or not.
Dr Ganguly: Volunteers after counseling and informed consent are randomised using a computer, according to age, sex, ethnic group, comorbidities, and similar sampling is done in both groups. They may be followed for up to two years or at least six months for the placebo. But at the end of the trial, they should be provided with the vaccine.
Q. What test can be done to know about the safety and effectiveness of a vaccine?
Dr Jameel: Safety and efficacy is determined in trials. Phase 1 tests safety in a small healthy volunteer group (20-50 people) and any adverse events are recorded. Whether the vaccine induces antibodies or not is also checked (called immunogenicity). Phase 2 expands safety and immunogenicity in a much larger population (100-500 people).
Finally, Phase 3 tests efficacy. In this, thousands of volunteers (10,000+) are divided randomly into two groups—vaccine and placebo. At the end of the study, all volunteers are tested to see who got naturally infected, and then the code is broken to see how many of those are in the vaccine or placebo groups. This is used to calculate efficacy.
Let us assume 100 people got infected—90 in the placebo group and 10 in the vaccine group. This means the vaccine has an efficacy of 90%.
Dr Ganguly: Safety is monitored through adverse reaction and severe adverse reactions, either or both through volunteers or through cell phones. Efficacy is through freedom from disease or freedom from the infection.