Is Flesh-Eating Bacteria That Disfigure the Body Likely to Spread in Australia?
Flesh-eating bacteria, a term that sends chills down the spine, refers to a group of bacteria that can cause severe infections, rapidly destroying skin, muscle, and other soft tissues. While cases of infections caused by these bacteria have been reported globally, the question arises whether this dangerous condition is likely to spread in Australia. With climate change, increasing international travel, and various environmental factors, the risk of infections due to flesh-eating bacteria may be influenced by multiple factors. This article aims to explore the nature of flesh-eating bacteria, how they spread, the potential for these infections to affect Australians, and what steps can be taken to prevent them.
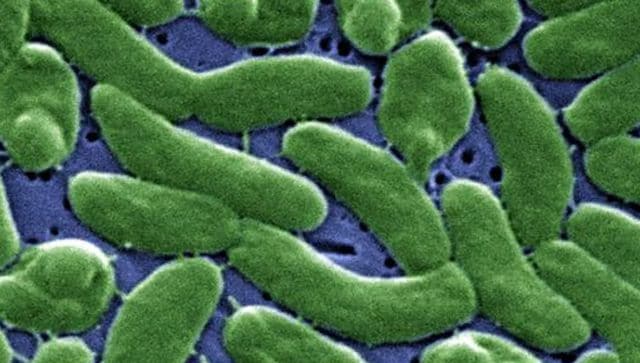
Flesh-eating bacteria is a layman’s term commonly used for necrotizing fasciitis, a life-threatening infection that rapidly destroys tissue, often leading to disfigurement or even death if not treated swiftly. The condition occurs when bacteria infect the soft tissue, including skin, fat, and muscle. The most common culprits of this infection are:
These bacteria thrive in environments that support rapid growth, especially when they enter the body through cuts, scrapes, or punctures. The infection often begins suddenly, with symptoms worsening within hours. Severe pain, fever, and swelling are common, and the infection can spread rapidly, sometimes leading to organ failure.
Flesh-eating bacteria can be transmitted through several pathways, and understanding these transmission routes is critical to assessing the potential for these infections to spread in any region, including Australia.
Australia, with its diverse climate and extensive coastline, presents unique conditions that could affect the spread of flesh-eating bacteria. While the occurrence of necrotizing fasciitis in the country is relatively low compared to other regions, certain factors could contribute to an increased risk.
Australia’s coastal regions, especially in the warmer northern parts, are already seeing an increase in the incidence of Vibrio vulnificus infections, which are associated with warmer seawater. These infections can be severe, particularly in individuals who have compromised immune systems or underlying chronic conditions.
Additionally, with the increase in global tourism, travelers visiting Australian beaches could unknowingly introduce new strains of bacteria into the region, which could further spread the disease.
Although necrotizing fasciitis caused by flesh-eating bacteria is relatively rare in Australia, cases do occur. According to available data, most infections are linked to Group A Streptococcus (GAS) and Vibrio vulnificus. However, the number of cases is small compared to the overall population.
In the past decade, there have been sporadic reports of Vibrio vulnificus infections, particularly in warmer regions such as Queensland. These infections have been more common during the warmer months when seawater temperatures rise. While the total number of infections remains low, the rapid nature of the condition, along with its potential severity, makes it a serious health concern.
The Group A Streptococcus strain, responsible for many cases of necrotizing fasciitis, continues to be a more common cause of infection in Australia. It is often linked to trauma, including post-surgical infections, accidents, and sometimes insect bites or animal scratches. However, healthcare facilities and quick medical intervention have generally kept the cases in check.
Given the factors mentioned above, it is possible that Australia could see an increase in cases of flesh-eating bacteria. Climate change, warmer seawater temperatures, and an aging population could all contribute to more people being exposed to conditions where these infections could occur.
The potential rise in cases of Vibrio vulnificus infections, in particular, warrants close attention. Coastal communities, as well as international tourists visiting Australia’s beaches, could unknowingly be exposed to these bacteria. Moreover, as the bacteria thrive in warm seawater, regions experiencing hotter-than-usual temperatures may see an uptick in cases.
Additionally, healthcare professionals in Australia must remain vigilant about Group A Streptococcus infections, particularly in hospitals or healthcare settings where surgical wounds and trauma could lead to infections. Early detection, proper wound care, and quick antibiotic treatment are essential to prevent the rapid spread of infection.
Preventing the spread of flesh-eating bacteria requires a multifaceted approach. Here are a few strategies:
While the spread of flesh-eating bacteria in Australia is not a major epidemic at present, there are several factors—rising temperatures, increased exposure to seawater, and the growing population of immunocompromised individuals—that could increase the risk of these infections. Although rare, the severity and speed with which flesh-eating bacteria can cause damage make it a significant health concern. Vigilance, education, and prompt medical intervention will be crucial in preventing outbreaks and minimizing the risks posed by these dangerous infections. With proper precautions, Australians can enjoy their outdoor activities while keeping these life-threatening infections at bay.